services

Our experienced staff will assist with the following in a Managed Care Claim Review:
• Analyze existing contracts to identify deficiencies.
• Determine the correct reimbursement due from Managed Care contracts.
• Provide recommendations for enhancing and maximizing revenue per contract language.
• Facilitate collections by review of current billing issues and denials.
• Recover lost dollars due from existing Managed Care Contracts

Outsourcing A/R (90) ninety days and over will:
• Decrease backlog by allowing staff time to reorganize and prioritize their current work.
• Provide management the flexibility to recruit appropriate personnel to fill vacant positions.
• Identify causes of non-payment, eliminating extensive staff research time.
• Recommend procedures to improve billing accuracy.
• Re-bill, if necessary, to appropriate insurance carrier.
All Services are Individually Tailored to Meet Your Specific Needs.
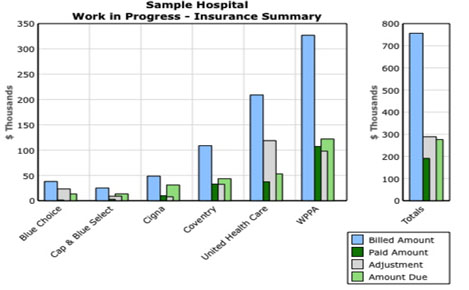
Detailed monthly management reports will be generated for each service. Charts and graphs will be provided to illustrate potential problems.
|
 |
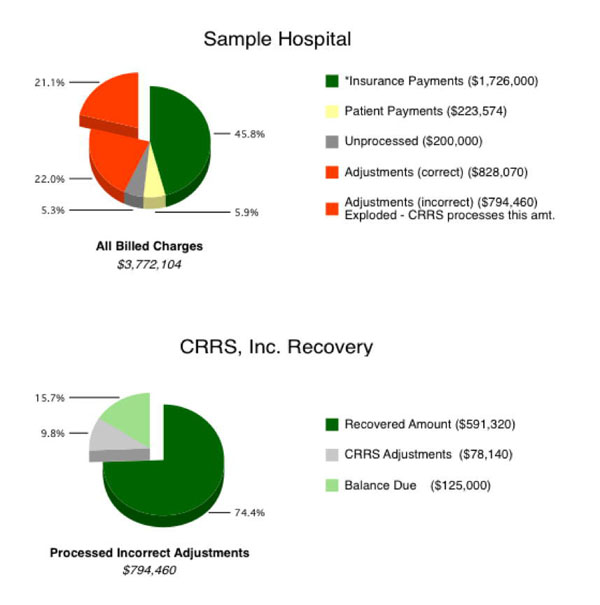
Example of What We Offer
These graphs show exactly how much is recovered. The two red slices represent hospital adjustments.
CRRS disputes the incorrect adjustments shown as exploded in the top graph. The bottom graph shows the results of CRRS working with this amount.